STAY COVERED & BE INFORMED
Prepare for Medicaid Eligibility Unwinding
At the beginning of the COVID-19 pandemic, the federal government declared a public health emergency or PHE. Since March 2020, Guam Medicaid has followed special requirements related to the federal COVID-19 Public Health Emergency (PHE). These requirements have allowed Guam Medicaid participants to be continuously enrolled throughout the COVID-19 Public Health Emergency (PHE), and this “protected group” were allowed to remain on Medicaid regardless of any changes to their eligibility status.
However, on December 23, 2022, Congress passed the FY 2023 Consolidated Appropriations Act (CAA) that ends the continuous enrollment requirement for Medicaid that requires the State Medicaid agencies to begin renewals to redetermine eligibility.
This website will be updated periodically. Information is current as of May 16, 2023.
DON’T RISK A GAP IN YOUR MEDICAID COVERAGE
What does this mean?
- Guam Medicaid will begin this unwinding process during the month of May 2023 and is required to complete this process no later than July 2024. This will allow sufficient time for redetermining eligibility by assigned groups and to ensure that medical coverage for Medicaid participants is not disrupted.
- Guam Medicaid will conduct these redeterminations based on groups and plans to conduct this process whereby the highest utilizers of Medicaid will be redetermined toward the end of the 12-month unwinding period.
- Guam Medicaid participants who are also recipients of cash assistance and/or the Supplemental Nutrition Assistance Program (SNAP) who have submitted their Simplified Renewal Forms (SRF) do not need to resubmit another SRF strictly for Medicaid.
- New or reopen applications are considered separate from the protected group and will follow the normal enrollment and eligibility requirements. For example, if a new applicant did not meet the income eligibility requirement, that applicant would be denied.
Starting May 2023 and over the next 12-month period
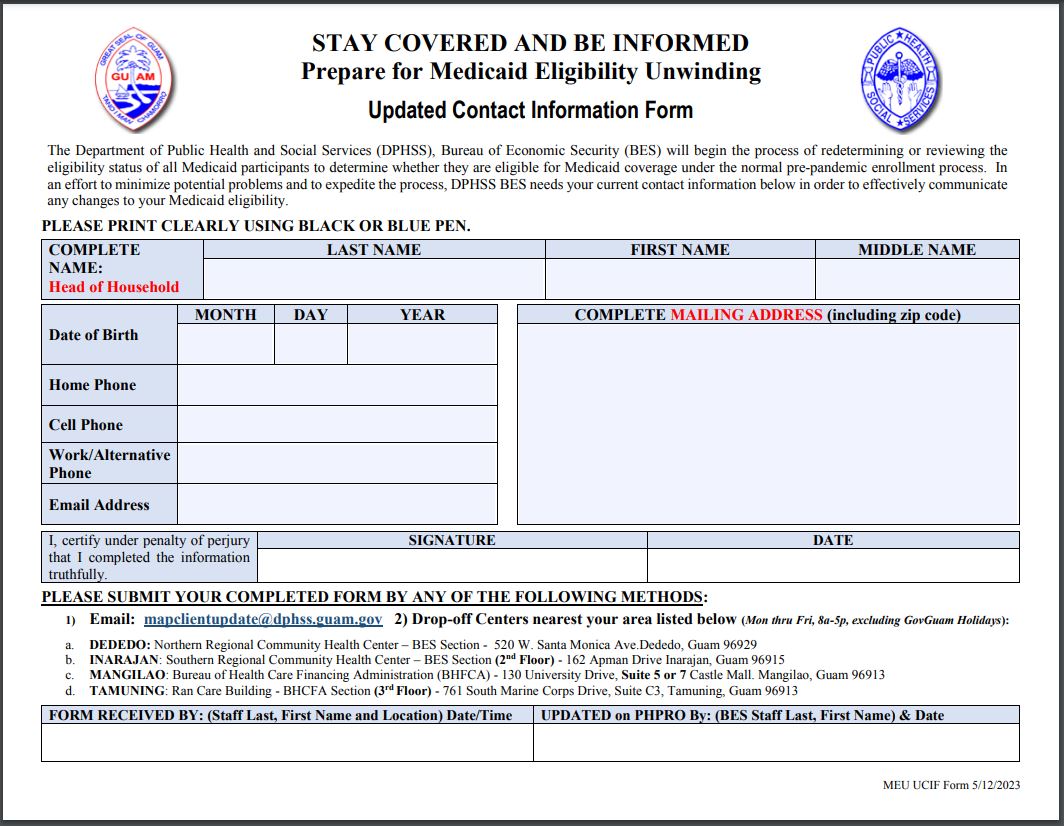
The Department of Public Health and Social Services (DPHSS) will begin Guam Medicaid’s “Unwinding Period” to redetermine all Medicaid participants’ eligibility coverage to determine whether they are eligible for Medicaid under the normal pre-pandemic enrollment process. In an effort to minimize potential problems and to expedite the process, DPHSS BES will require all Medicaid beneficiaries to complete an Updated Contact Information Form.
UPDATE YOUR CONTACT INFORMATION
How to submit your Updated Contact Information Form
1. Email: mapclientupdate@dphss.guam.gov
2. Drop-off Centers nearest your area listed below (Monday thru Friday, 8am-5pm, excluding GovGuam Holidays):
DEDEDO
Northern Regional Community Health Center – BES Section
520 W. Santa Monica Ave.
Dededo, Guam 96929
Tel: (671) 635-7432 / 7485
INARAJAN
Southern Regional Community Health Center – BES Section
(2nd Floor)
162 Apman Drive
Inarajan, Guam 96915
Tel: (671) 828-7542
MANGILAO
Bureau of Health Care Financing Administration (BHFCA)
130 University Drive, Suite 5 or 7 Castle Mall
Mangilao, Guam 96913
Tel: (671) 735-7475
TAMUNING
Ran Care Building – BHCFA Section (3rd Floor)
761 South Marine Corps Drive, Suite C3
Tamuning, Guam 96913
Tel: (671) 300-7330




Frequently Ask Questions
What is Medicaid Eligibility Unwinding?
At the beginning of the COVID-19 pandemic, the federal government declared a public health emergency or PHE. Since March 2020, Guam Medicaid has followed special requirements related to the federal COVID-19 Public Health Emergency (PHE). These requirements have allowed Guam Medicaid participants to keep their health coverage, even if they no longer qualify under the guidelines due to higher income or changes in eligibility.
However, on December 23, 2022, Congress passed the FY 2023 Consolidated Appropriations Act (CAA) that ends the continuous enrollment requirement for Medicaid and starts renewals to redetermine eligibility.
Starting May 2023 and over the next 12-month period, the Guam Medicaid program under the Department of Public Health and Social Services – Bureau of Economic Security (BES) will begin its redetermination of all Medicaid participants’ eligibility coverage.
What do I need to do?
If you moved during the pandemic or if any of your contact information changed such as, your phone number, mailing address or email, please fill out an Updated Contact Information Form. This form is available online at the following link: https://dphss.guam.gov/wp-content/uploads/2023/05/Guam-Medicaid-Unwinding-Contact-Form.pdf.
What will happen if I don’t update my contact information during the “unwinding” period?
Your Medicaid coverage might be terminated because an Eligibility Specialist (case worker) was unable to contact you.
What if my current information status is the same within the past year, do I need to submit an updated contact information form?
Yes, we still require that you fill out and submit the Updated Contact Information Form regardless if there were no changes.
What will happen if I am no longer eligible for Medicaid due to my income?
Check with your employer on how you can enroll to the group health plan because losing Medicaid coverage is a qualifying event which allows you to enroll outside of the Open Enrollment Period.
What documents will I need in order to enroll in my employer’s group health plan?
DPHSS BES will provide you the TERMINATION OF COVERAGE letter that you need to attach to your group health plan enrollment form.
Is there a deadline to enroll in my employer’s group health plan?
Yes, you will have to enroll in your employer’s group health plan within 30 days from the date of termination of your Medicaid coverage.
What if I have already submitted the Simplified Renewal Form (SRF) for Cash Assistance and/or Supplemental Nutrition Assistance Program (SNAP), will I need to submit another SRF for Medicaid?
No. Only one (1) Simplified Renewal Form (SRF) is needed if you are receiving Cash Assistance, Supplemental Nutrition Assistance Program (SNAP), and/or Medicaid.
If I get terminated for Medicaid, how can I file for an appeal?
You can request a Fair Hearing by calling or visiting:
The Bureau of Management Support (BMS)-Unit #15
130 University Drive
Mangilao, Guam 96913
(671) 735-7344 / 7256
Is there a deadline to file an appeal also known as a Fair Hearing?
Yes, you can ask for a fair hearing anytime up to 90 days following the date of notice.
How soon will I be notified about my Medicaid coverage?
As soon as your case is redetermined you will receive a Notice of Action. The redetermination will take place starting May 2023 and continue over the next 12-month unwinding period.
If I have unpaid medical bill(s) that I think should be covered by the Medicaid program, who can I contact?
You may drop your unpaid medical bill(s) at the Bureau of Health Care Financing Administration office at their Tamuning location listed below.
Upon submission, please provide your full name, contact number, case number, and date of birth.
Bureau of Health Care Financing Administration
Ran Care Building
BHCFA Office (3rd Floor)
761 South Marine Corps Drive, Suite C3
Tamuning, Guam 96913
Tel: (671) 300-7330